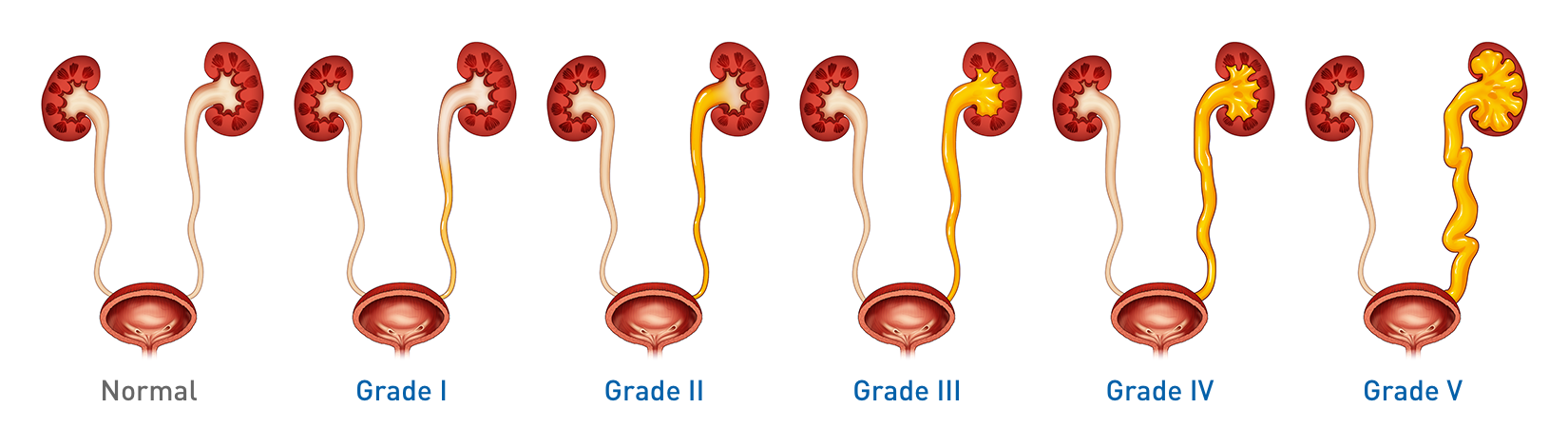
Urinary reflux diagnosis and grading scale
A VUR diagnosis usually comes after a febrile UTI is confirmed
When a child presents with a febrile urinary tract infection (fUTI), it could indicate vesicoureteral reflux (VUR), commonly referred to as urinary reflux.
VUR is most often detected as a result of diagnostic investigations of fUTI or of hydronephrotic (distended) kidney. It may also be suspected in children presenting with high blood pressure or kidney insufficiency.
Diagnosing VUR
Accurate diagnosis and grading of VUR can help with the implementation of individualized treatment plans. Diagnosis requires a micturating cystourethrogram (MCUG), typically performed by a radiologist equipped for the fluoroscopy and catheterization of children.
As a result of MCUG assessment, any VUR will be graded from I to V based on the dilation of the ureter and presence and degree of distortion of renal structures.
Imaging Procedures after first UTI per the 2010 American Urologic Association (AUA) guidelines for the management and screening of primary vesicoureteral reflux in children:3
- Recommendation: Perform a renal and bladder ultrasound (RBUS) to assess the upper urinary tract
- Option: DMSA (technetium-99m-labeled dimercaptosuccinic acid) renal imaging can be obtained to assess the status of kidneys for scarring and function
If the RBUS is normal, the AUA does not recommend proceeding with a MCUG.
In 2011, the American Academy of Pediatricians presented an update to the clinical practice guidelines for the diagnosis and management of the initial UTI in febrile infants and children 2-24 months. In the updated guidelines, MCUG is only indicated if renal and bladder ultrasonography (RBUS) reveals hydronephrosis, scarring or other findings suggesting either high-grade VUR or obstructive uropathy.4
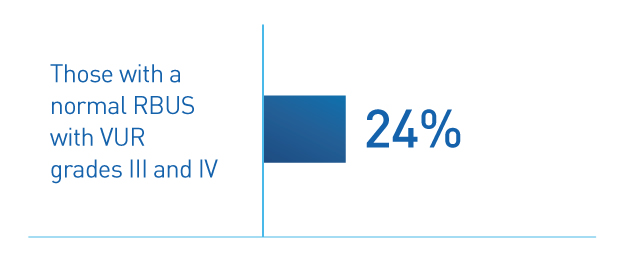
However, a 2013 study of children with their first UTI and normal RBUS shows that in 24% of patients, VUR would not have been detected.5 The same study shows that 15% of these children had recurrent pyelonephritis and 7% went on to surgical intervention.5