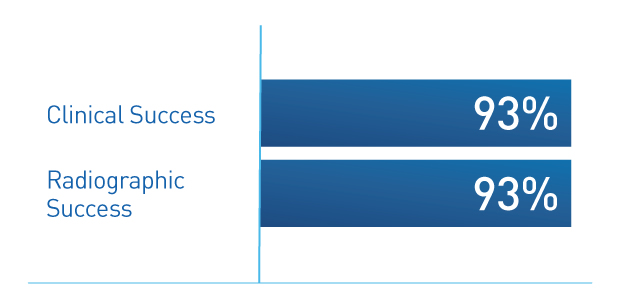
54 children ages 7 months to 16.6 years (mean age 4.1 years) underwent Deflux treatment using the Double HIT technique, with an average follow-up of 19 months and a MCUG 1 year after treatment. Radiographic success was defined as a negative MCUG at 1 year; clinical success was defined as no febrile UTIs at 1 year.
8.4 years median follow-up shows high Deflux efficacy and parental satisfaction2
89.2% clinical success – with no reported fUTI post-Deflux treatment
94.1% total patient satisfaction with Deflux:
- 94.1% highly satisfied
- 2.4% partially satisfied
- 3.5% dissatisfied
575 patients underwent Deflux injection for VUR between 2008-2012. 99 of these patients’ parents were successfully contacted and interviewed. Median follow-up time from surgery was 8.4 years. 83 families reported at least 1 fUTIs pre-operatively. Of these, only 9 (10.8%) reported fUTIs post-operatively, for an overall clinical success rate of 89.2%. Clinical success was 93.1% in patients whose pre-operative fUTIs were treated outpatient and 80% in those hospitalised at least once for fUTI treatment pre-operatively.
15-25 years follow-up shows durable and effective results for grade IV VUR3
A long-term study (15-25 year follow up) concluded Deflux as a viable option for patients with grade IV VUR, including those with double ureters.
- 75% of patients did not need ureteral reimplantation
- Optimal injection technique and higher injection volume were associated with a reduced ureteral reimplantation rate
- Low risk of late clinical occurrence (UTI, persistent VUR or need for open surgery)
- 97% free from safety issues
185 patients were included in the study; 237 grade IV VUR ureters were treated. All study patients were diagnosed with VUR after pyelonephritis. Among patients treated during the second 5-year period compared with the first, there was a significant decrease in the rate of ureteral reimplantation (31% vs. 16%, p=0.0365). The difference may be attributable to developments over time in injection technique.
The Double HIT is the most common injection technique:
The STING technique is a subureteric injection in which the needle is placed directly below the ureteral orifice at the 6 o’clock position.4
The HIT technique is a single intra-ureteric injection technique that is a modification of STING.4
The Double HIT technique is a refinement of the STING and HIT procedures and includes both proximal and distal intra-ureteric injections.4 A 2014 study shows, the Double HIT technique is the most commonly performed technique for correction of VUR by paediatric urologists in the U.S.5 In that study 92% of Deflux procedures use the Double HIT technique which has demonstrated higher efficacy rates.5
Optimal placement and higher injection volumes are associated with improved success.3,5
See how paediatric urologists administer Deflux
Deflux should only be administered by qualified surgeons experienced in the use of a cystoscope and trained in subureteral injection procedures and must not be injected intravascularly as injection into blood vessels may cause vascular occlusion.
Please refer your appropriate patients with vesicoureteral reflux (VUR) to a paediatric urologist upon VUR diagnosis.